How TRT Protocols Are Designed (Dose, Frequency, Labs, Adjustments)
- Primal Pulse Team
- Jan 23
- 6 min read
Testosterone replacement therapy protocols are often described online as if they are endlessly customizable or based on personal preference. In reality, competent clinics design and adjust TRT using a small number of repeatable decision rules. Most confusion comes from not understanding what decision a given lab, dose, or adjustment is meant to inform.
This article explains how TRT protocols are actually designed and modified in clinical practice, focusing strictly on dose, frequency, labs, and adjustments.
The First Constraint: Consistency Before Optimization
Before any protocol can be evaluated or adjusted, clinics first lock in consistency.
Bloodwork is not an absolute truth. It is a snapshot taken at a specific point in a dosing cycle. The value of that snapshot comes from being comparable to previous snapshots taken under the same conditions.
This is why clinics insist on stable dose, stable frequency, and repeatable lab timing before making changes. If any of those variables move at the same time, the lab result cannot be interpreted reliably.
The goal of early TRT management is not optimization. It is to create a stable reference point so future changes can be evaluated meaningfully.
This is why patients are often told to wait, even if they feel impatient. Waiting is not inaction. It is preserving signal.
How TRT PROTOCOLS CHOOSE THE Starting Dose
Most clinics start TRT at a conservative to moderate dose. This is intentional.
A starting dose is not meant to be perfect. It is meant to answer two questions:
First, does restoring testosterone into the normal range improve symptoms at all.
Second, does the patient show early safety signals such as rising hematocrit or blood pressure.
Clinical guidelines recommend using the lowest dose that brings testosterone into the mid normal range rather than pushing levels high from the start.
Starting lower allows clinicians to increase dose if needed, while watching for side effects that would otherwise be masked by aggressive dosing.
A patient who improves meaningfully on a modest dose has demonstrated sensitivity. A patient who does not improve may need either a higher dose or reassessment of whether testosterone is the real driver of symptoms.
How Injection Frequency Is Chosen
Injection frequency is often misunderstood as an optimization tool. In clinical practice, it is a stability tool.
Weekly injections are the default for most patients because they balance convenience, adherence, and reasonably stable testosterone exposure.
More frequent injections are introduced when a specific problem appears, most commonly large swings between post injection highs and pre injection lows that correlate with symptoms.
Daily injections are not standard. They are reserved for patients who are particularly sensitive to fluctuations or who cannot tolerate higher peak levels.
Importantly, frequency is not adjusted to chase estradiol numbers or internet rules. It is adjusted to reduce variability when variability is clearly the problem.
Clinics generally want to understand dose response first before modifying frequency, because changing frequency too early makes it harder to learn how the patient responds to testosterone itself.
How Labs Are Scheduled and What They Represent
Labs are scheduled to answer specific questions, not to capture perfect physiology.
For injectable testosterone, clinics want to understand average exposure or trough exposure depending on their monitoring philosophy. Some guidelines recommend mid interval testing for weekly injections to approximate average levels, while many clinics use trough testing for practicality and consistency.
For daily injections or transdermal therapies, labs are drawn after steady state is reached and at a consistent time after dosing, because levels fluctuate less across the day once absorption stabilizes.
The key principle is not peak versus trough. It is repeatable timing relative to dosing.
If lab timing changes, the meaning of the number changes. This is why consistent timing matters more than theoretical precision.
Shift work does not invalidate labs. As long as the draw is consistently timed relative to the patient's dosing and sleep cycle, trends remain interpretable.
How Testosterone Levels Are Interpreted
Clinics do not treat a testosterone number in isolation.
A total testosterone value is interpreted alongside symptoms, safety labs, and dosing context. The commonly cited target range of roughly 450 to 600 ng/dL reflects a middle of the normal range where benefits are expected without unnecessary risk, not a hard goal for every patient.
If levels are below target and symptoms persist, dose or frequency may be increased.
If levels are above target, dose is reduced even if the patient feels subjectively well, because long term risk increases without clear added benefit.
If levels are normal but symptoms do not improve, clinicians do not automatically increase dose indefinitely. Instead, they reassess whether symptoms are truly androgen mediated.
What Each Lab Actually Tells Your Clinic
Understanding what each test measures helps you have more informed conversations with your provider about your protocol.
Lab Test | What It Tells Your Clinic | Why It Matters for Protocol Decisions |
Total Testosterone | Whether dose is achieving target range | Guides dose increases or decreases |
Free Testosterone | Bioavailable testosterone (checked if SHBG is abnormal) | Explains why two patients at same total T feel different |
SHBG | How much T is bound versus available | Changes interpretation of total T levels |
Hematocrit | Red blood cell concentration | Hard safety limit that may require dose reduction |
PSA | Prostate health screening | Monitors for concerning changes, not routine cancer screening |
Estradiol | Only checked if symptoms present | Not routinely monitored; only matters if gynecomastia or edema appears |
How Dose Adjustments Are Made
Dose adjustments are diagnostic.
Increasing dose tests whether symptoms are testosterone responsive.
Decreasing dose tests whether side effects are dose dependent.
Clinics adjust one variable at a time whenever possible. Changing dose and frequency simultaneously destroys the ability to interpret cause and effect.
Adjustments are incremental, not dramatic, because testosterone effects and downstream markers such as hematocrit respond over weeks, not days.
If symptoms improve with dose increases but safety markers worsen, the protocol has reached a practical ceiling.
If symptoms do not improve despite normal testosterone levels, continued escalation is not justified.
Where SHBG Fits Into Protocol Design
Sex hormone binding globulin affects how testosterone is interpreted, not how labs are timed.
SHBG binds testosterone in the blood. Higher SHBG means less free testosterone for a given total level. Lower SHBG means more free testosterone.
Clinics use SHBG to explain why two patients with the same total testosterone feel different, and to decide whether free testosterone should be evaluated.
SHBG does not dictate injection frequency rules on its own. It modifies interpretation and dosing targets.
A helpful mental model is that SHBG is a lens, not a lever.
Estradiol and Why It Rarely Drives Protocol Changes
Estradiol rises during TRT because some testosterone converts into estrogen. This is expected and often beneficial.
Clinical guidelines do not recommend routine estradiol monitoring unless the patient has symptoms such as gynecomastia or significant fluid retention.
Clinics do not chase estradiol numbers. They treat symptoms.
When estrogen related symptoms appear, the first intervention is lowering the testosterone dose, which reduces estrogen production at the source.
Aromatase inhibitors are not routinely used because suppressing estrogen can harm bone density and does not reliably improve outcomes.
Blood estradiol levels do not directly represent tissue effects. This is why labs alone are not used to justify aggressive estrogen management.
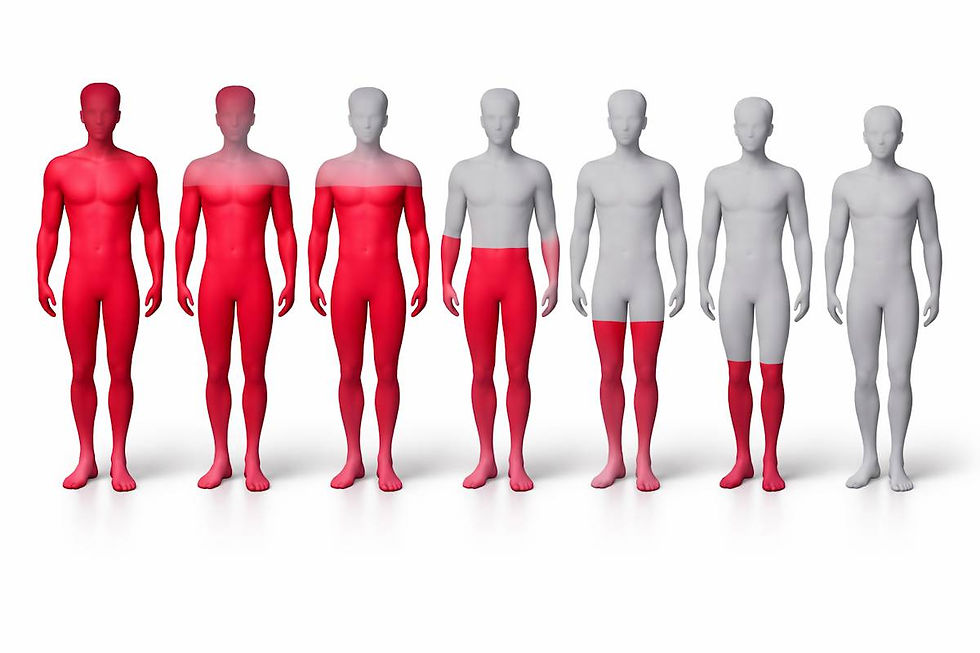
Hematocrit, Ferritin, and Hard Safety Limits
Hematocrit is one of the few parameters that can force protocol changes regardless of symptoms.
Testosterone stimulates red blood cell production. If hematocrit rises too high, blood viscosity increases and clot risk becomes a concern.
Guidelines are clear that hematocrit at or above 54 percent requires intervention, usually temporary cessation or dose reduction.
Levels in the low 50s prompt closer monitoring or dose adjustment.
Phlebotomy can reduce hematocrit quickly, but repeated blood removal depletes iron stores. This can lead to low ferritin, fatigue, and paradoxical problems even if hematocrit remains elevated.
Because of this tradeoff, many clinics prefer dose reduction or modality change before relying on repeated phlebotomy.
Hematocrit does not get optimized. It limits how aggressive a protocol can be.
How Often Protocols Are Revisited
TRT changes are slow because biology is slow.
Injectable testosterone takes weeks to reach steady state. Hematocrit changes lag even further behind dose changes.
This is why clinics often wait six to twelve weeks between adjustments unless a clear safety issue appears.
If a patient shows no meaningful improvement after several months with normal testosterone levels, clinicians reassess the diagnosis and may discontinue therapy rather than escalate endlessly.
TRT is not meant to override unrelated health issues. It is meant to correct a specific deficiency.
Evaluating TRT Clinic Competence
Understanding how protocols should be designed helps you assess whether a clinic follows evidence-based practices or cuts corners.
Aspect | Red Flag (Poor Practice) | Green Flag (Evidence-Based) |
Starting approach | Starts everyone at same dose, never adjusts | Starts conservative, monitors response, adjusts based on individual labs and symptoms |
Estradiol management | Automatically prescribes AI from day one | Only addresses E2 if symptoms appear; first tries dose adjustment |
Lab timing | Changes timing between tests or does not explain why timing matters | Consistent timing; can explain rationale for chosen timing |
Hematocrit response | Ignores rising Hct or recommends indefinite phlebotomy | Discusses dose reduction, modality change, or investigates sleep apnea before serial phlebotomy |
Frequency changes | Changes frequency and dose simultaneously | Adjusts one variable at a time to understand cause and effect |
When symptoms do not improve | Keeps increasing dose indefinitely | Reassesses diagnosis after 6 to 12 months if no response to normalized T |
Next Steps
Well-designed TRT protocols are not mysterious and they are not fragile.
They are built around consistency, cautious escalation, clear safety thresholds, and disciplined interpretation of labs.
Most confusion comes from mixing rules that were meant for different decisions.
Once the underlying logic is understood, TRT becomes easier to evaluate and easier to discuss with a clinician in concrete terms.