Bloodwork for TRT: Which Labs You Actually Need (And Which Ones You Don't)
- Primal Pulse Team
- 4 days ago
- 6 min read
Bloodwork answers two questions: Is low testosterone the real problem? Once TRT starts, is it working safely? Most confusion comes from mixing these phases.
In this Primal Pulse guide, we explain which labs matter, when to draw them, and what each one changes in actual clinical decisions.
Phase A: Diagnostic BLOODWORK FOR TRT (BEFORE STARTING)
TRT treats confirmed hypogonadism, not vague fatigue or low motivation.
Symptoms like low energy, low libido, brain fog, weight gain, and low mood overlap heavily with thyroid disease, insulin resistance, sleep disorders, and anemia.
Clinical guidelines emphasize confirming low testosterone and evaluating for secondary or reversible causes before starting TRT.
Lab Test | Purpose | What It Rules Out | When to Skip |
Total Testosterone (2x) | Confirm persistent low T | Temporary fluctuation from stress/illness | Never |
TSH (+ Free T4 if abnormal) | Screen thyroid function | Hypothyroidism causing similar symptoms | Never |
CBC | Check for anemia, baseline hematocrit | Anemia-related fatigue | Never |
A1C or Fasting Glucose | Screen metabolic health | Diabetes, insulin resistance | Never |
LH and FSH | Identify cause of low T | Pituitary disorders, reversible causes | Sometimes (provider discretion) |
Prolactin | Screen pituitary function | Prolactinoma, pituitary tumors | Only if symptoms suggest it |
Total Testosterone
Two early morning tests on separate days confirm persistent deficiency, not a temporary dip from stress, illness, or poor sleep.
Most guidelines define low testosterone around 300 ng/dL, but diagnosis requires both low levels and symptoms.
Clinical decision: Confirms whether testosterone deficiency is real and persistent.
Thyroid Screen (TSH, then Free T4 if abnormal)
Hypothyroidism is common and causes many of the same symptoms as low testosterone. Low thyroid function can also suppress testosterone levels secondarily.
CDC and major endocrine bodies recognize hypothyroidism as a frequent cause of fatigue, weight gain, and hormonal disruption.
Clinical decision: If thyroid disease is present, treating it often improves symptoms and testosterone without TRT. Skipping this step leads many people into unnecessary long term hormone therapy.
CBC (Complete Blood Count)
Screens for anemia that can cause fatigue independent of testosterone, and establishes baseline hematocrit before TRT. Baseline hematocrit is critical because TRT commonly raises red blood cell levels later.
Clinical decision: Identifies non hormonal causes of symptoms and sets safety reference for monitoring.
A1C or Fasting Glucose
Insulin resistance and diabetes are strongly linked to fatigue, low libido, and low testosterone. Low testosterone is common in men with metabolic syndrome and obesity.
Clinical decision: If metabolic disease is driving symptoms, addressing it improves outcomes and sometimes raises testosterone naturally.
LH and FSH
These pituitary hormones distinguish primary hypogonadism (testes not responding) from secondary hypogonadism (brain signaling problem). Guidelines recommend measuring them when diagnosing testosterone deficiency.
Clinical decision: Guides further evaluation and identifies reversible or treatable causes such as pituitary disorders.
Prolactin (Select Cases)
High prolactin can suppress testosterone production and signal pituitary tumors, which are rare but important.
Clinical decision: If elevated, further evaluation replaces TRT escalation.
The diagnostic gate: TRT makes sense when testosterone is consistently low, symptoms fit hypogonadism, and simpler causes have been ruled out or treated. If a clinic skips this phase and jumps straight into TRT, that is a red flag.
Phase B: Monitoring Labs (Once TRT Begins)
Once TRT starts, the goal shifts to confirming testosterone is in range and the body is tolerating it safely. These labs are routinely sufficient for most patients.
Core Monitoring Panel
Almost always needed:
Total testosterone and free testosterone (or calculated if SHBG available), CBC with hematocrit and hemoglobin, PSA (age and risk dependent), comprehensive metabolic panel (liver and kidney markers), lipid panel, A1C or fasting glucose (periodic).
Ordering far beyond this routinely rarely improves outcomes.
What Each Core Lab Actually Changes
Total Testosterone
Confirms TRT is achieving physiologic levels. Target is typically mid normal range, often roughly 450 to 600 ng/dL, per guidelines. Low levels trigger dose increase. High levels trigger dose reduction.
Free Testosterone and SHBG
Explains symptom mismatch when total testosterone looks normal. High SHBG means less biologically active testosterone. Low SHBG means more free testosterone for a given total. This guides interpretation and dosing targets.
CBC (Hematocrit)
Monitors TRT induced red blood cell increase. Guideline threshold is hematocrit 54 percent, which requires intervention. Actions include dose reduction, temporary pause, or phlebotomy.
PSA
Screens prostate response. Guidelines advise urology referral if PSA rises more than 1.4 ng/mL in first year or exceeds 4.0 ng/mL. Pause TRT and evaluate if thresholds crossed.
CMP
General health monitoring. Injectable and transdermal testosterone are not hepatotoxic, but overall metabolic health matters.
Lipids and Glucose
Monitor cardiovascular and metabolic risk. TRT can slightly alter cholesterol patterns and body composition.
Why Mid Range Matters
The target range of 450 to 600 ng/dL balances symptom relief against side effects. Most men experience resolution of hypogonadal symptoms in this range.
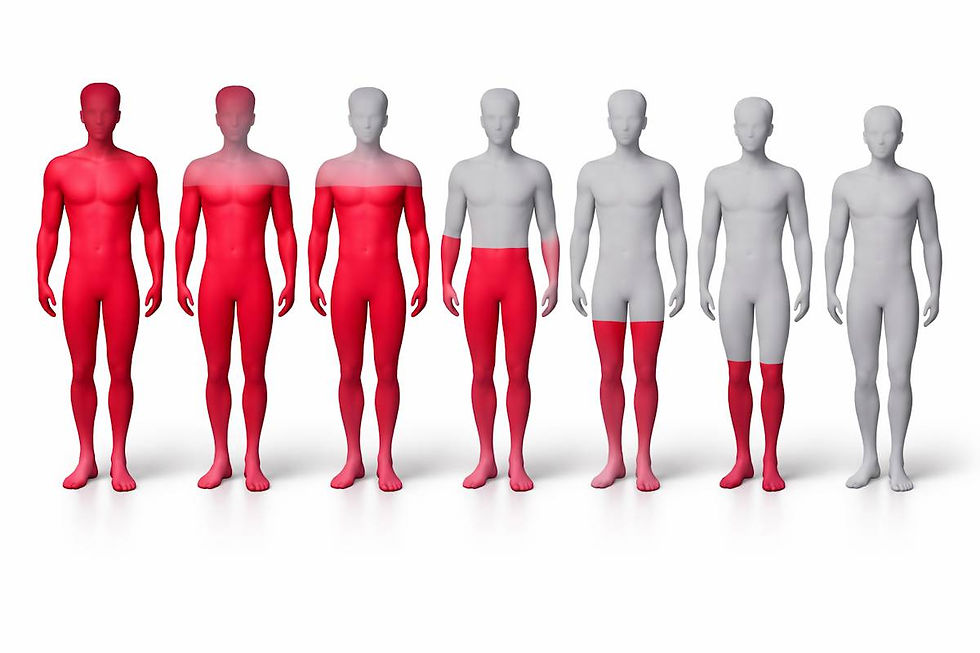
Pushing higher increases risk of polycythemia (elevated red blood cells), sleep apnea worsening, and potential cardiovascular strain without additional symptom benefit. Lower levels may not fully resolve symptoms.
The goal is not maximum testosterone but optimal testosterone for health and function.
Lab Timing Rules
The goal is not perfect physiology. The goal is repeatable reference points.
Injectable Testosterone
For weekly injections, draw at trough (right before next injection) for consistency. This represents your lowest point and makes results comparable over time. Some clinicians prefer midway between injections to estimate average exposure, but trough is the standard for monitoring stability.
For split or daily injections, draw at the same consistent point relative to dosing each time.
Transdermal Gels or Creams
Draw several hours after application once steady state is reached, and keep timing consistent.
The golden rule: If you change lab timing, you change what the number represents. Consistency matters more than chasing peak or trough theory.
Phase C: Troubleshooting Labs (When Symptoms or Safety Issues Arise)
These are not routine baseline labs. They become essential when specific scenarios occur. Most TRT patients will need at least one of these at some point.
Estradiol
Check only with symptoms such as nipple tenderness, gynecomastia, or significant fluid retention. Guidelines do not recommend routine monitoring.
First response is dose adjustment, not estrogen blockers.
Ferritin and Iron Studies
Triggered when hematocrit is high and blood donation or phlebotomy is used. Repeated blood removal can deplete iron stores and cause fatigue.
This scenario is extremely common among TRT patients with elevated hematocrit.
Thyroid and Prolactin Rechecks
Triggered when symptoms persist despite adequate TRT levels. These should have been checked in Phase A, but if symptoms do not improve on TRT, rechecking rules out missed or new thyroid dysfunction.
Fertility Testing
Semen analysis, LH, and FSH if pregnancy is a goal. TRT suppresses sperm production. This should be discussed before starting TRT if fertility matters.
Practical Lab Schedule
Timing | Labs to Draw | Why This Timing Matters |
Before starting TRT | Full Phase A diagnostic panel | Establish baseline and confirm diagnosis |
6-12 weeks after starting or dose change | Total T, Free T, CBC, PSA | First check that dose is working and safe |
3-6 months | Total T, Free T, CBC, CMP, Lipids, PSA | Comprehensive safety check |
Every 6-12 months (once stable) | Total T, Free T, CBC, CMP, Lipids, PSA, A1C | Ongoing monitoring for stable patients |
As needed | Estradiol, Ferritin, Thyroid | Triggered by specific symptoms or issues |
Before TRT: Full diagnostic workup as outlined in Phase A.
6 to 12 weeks after starting or changing dose: Testosterone levels, CBC, sometimes PSA.
3 to 6 months: Repeat safety labs.
Once stable: Every 6 to 12 months. More frequent if hematocrit or PSA issues arise.
Common Scenarios and What to Check
Symptom/Issue | Labs to Check | Most Likely Cause | Next Step |
No symptom improvement after 8-12 weeks | Total T, Free T, SHBG, TSH, A1C | Dose too low, thyroid issue, or metabolic problem | Adjust dose or treat underlying condition |
Nipple tenderness, gynecomastia | Estradiol, Total T | Estradiol too high or dose too high | Reduce dose first |
Fatigue despite good T levels | Ferritin, CBC, TSH | Iron deficiency from phlebotomy | Iron supplementation or reduce donation frequency |
Hematocrit above 54% | CBC, Ferritin | TRT-induced polycythemia | Dose reduction, phlebotomy, check iron |
Rising PSA | PSA, repeat PSA | Normal variation or prostate issue | Urology referral if crosses threshold |
Feeling nothing after 8 to 12 weeks: Check testosterone, free T, thyroid, glucose.
Hematocrit rising: Check CBC and ferritin.
Nipple tenderness or bloating: Check estradiol and testosterone level.
Fatigue after blood donation: Check ferritin.
PSA anxiety: Repeat PSA and consult urology if thresholds crossed.
What Good TRT Monitoring Looks Like
Good care uses a proper diagnostic workup before TRT, a small focused monitoring panel after TRT starts, consistent lab timing, clear action thresholds, and one variable adjustments.
Bad care skips diagnosis and floods patients with unnecessary labs.
Next Steps
Responsible TRT follows this sequence:
confirm testosterone deficiency properly
rule out simpler causes first
start TRT only when indicated
monitor with a focused consistent lab panel
adjust based on clear decision rules
If a provider jumps straight to testosterone without basics like thyroid testing, that is not personalized care. That is a shortcut, and shortcuts create most of the confusion people experience with TRT.
Explore high-quality testosterone for research use on Primal Pulse.